Our teleradiology workflow is based on systematic, near real-time analysis using Avicenna.AI’s tools for analyzing CT scan exams performed in our partner establishments, in both scheduled and emergency workflows.
In typically scheduled workflows, the radiologist’s interpretation can occur retrospectively, even after the patient has left the department. AI analysis serves as an initial assessment tool, providing essential support in identifying urgent cases and streamlining patient care. This initial AI analysis is crucial for prioritizing examinations and allowing for immediate interpretation by a radiologist when required.
Every alert generated by the AI is promptly validated by a radiologist, regardless of the examination workflow (scheduled or urgent), ensuring a reliable and precise diagnosis.
The integration of AI, especially in scheduled activities, facilitates real-time adaptation of patient care by prioritizing examination interpretation as needed.
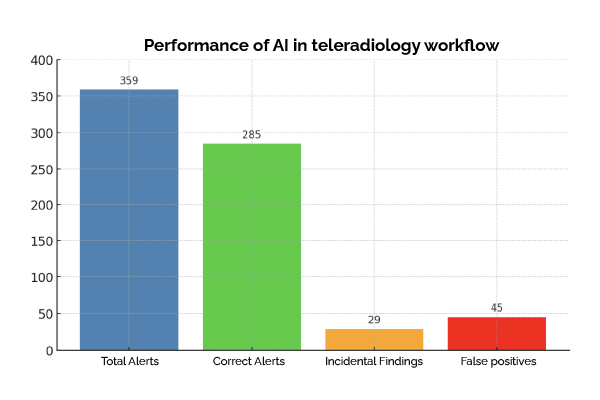
The graph below demonstrates the effectiveness of AI in this process, using statistics from a representative sample collected over one month of activity:
Key results
Overall reliability
The AI generated 359 alerts, most of which (285) were confirmed as correct. This underlines Avicenna’s AI’s effectiveness in identifying relevant real-time anomalies.
Incidental findings
29 alerts led to unexpected findings, demonstrating the value of exhaustive analysis in detecting secondary pathologies that are often overlooked. These findings considerably enrich our contribution to comprehensive patient care.
Managing false positives
The 45 false positives identified, mostly linked to technical artifacts (e.g. inadequate injection time), were corrected thanks to human review. This supervision ensures that patient care remains at the highest level of quality.
Enhanced workflow with AI
Integrating AI into our workflow has allowed us to achieve several key objectives:
- Improved Efficiency: Rapid identification of examinations that require special attention.
- Enhanced Quality: Expanded detection of anomalies, including unexpected findings.
- Resource Optimization: Reduced time required for the radiologist’s preliminary reading.
We are very pleased with the integration of Avicenna.AI into our teleradiology workflow. This demonstrates the concrete value of artificial intelligence as a complementary tool to human expertise, paving the way for faster, more accurate, and proactive healthcare
About TIM:
Founded in 2016, TIM is a committed company that positions itself as an essential partner in teleradiology for public and private healthcare institutions in France. Its mission is to provide and organize high-quality teleradiology services for scheduled activities and emergency PDS/CDS (day/night). TIM holds two Resah contracts for managing its activities (2022-055 lot 1 and lot 2). By offering a team of qualified experts and innovative technologies, TIM ensures fast and accurate diagnoses, making medical imaging accessible everywhere, for everyone.
Press contact:
Cédric MUNSCHY
Commercial Director
+33 (0)2 85 52 90 60 / communication@teleimagerie.net